先进的成像和手术技巧确保成功sful Removal of a Parathyroid Adenoma
 When Joselyn Lee’s calcium levels were high in 2018, her endocrinologist referred her toKunal Jain, MD, a head and neck cancer surgeon in the Department of Otorhinolaryngology at McGovern Medical School at UTHealth, who also specializes in parathyroid surgery.
When Joselyn Lee’s calcium levels were high in 2018, her endocrinologist referred her toKunal Jain, MD, a head and neck cancer surgeon in the Department of Otorhinolaryngology at McGovern Medical School at UTHealth, who also specializes in parathyroid surgery.
“But I didn’t have any symptoms, so I put off the surgery,” says Lee, who is 67. “Then in 2020, I started having some issues. I couldn’t tolerate heat and was always sweating. When I walked the dog, I’d be as wet as if I had been swimming. Some mornings I’d have dizziness, and I was always hungry and snacking. I have a good memory, and suddenly my memory wasn’t that great anymore. I would start making a sandwich and walk away and forget it.”
When Lee saw Dr. Jain in his office, she was apprehensive and scared. “I told him I had decided to go ahead with the surgery because of my symptoms, and that I had read online that the parathyroid glands are close to an important nerve and I was worried. He looked so young, but then he told me he’d done more than 100 of these procedures with no problems. His demeanor put me completely at ease. When I left his office, I felt confident and was ready to have the surgery then and there.”
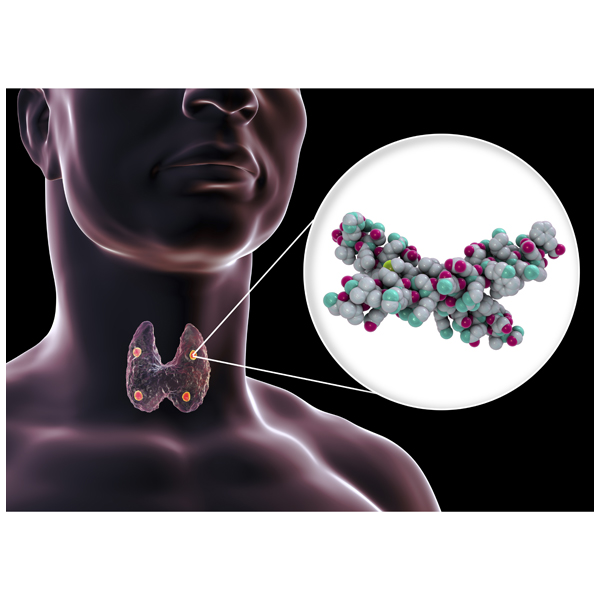
Dr. Jain took Lee to the OR in September 2020. “Usually one of the four parathyroid glands is secreting too much hormone. Excision of a parathyroid adenoma is a tricky operation, but when done well, patients experience a dramatic improvement in quality of life,” he says. “She was very nervous, but the surgery was extremely smooth. We used two types of imaging studies – SPECT-CT and in-office ultrasound to confirm the location. Her surgery took 30 minutes, done through a small 2 to 3 centimeter incision. Having the technology available to locate the malfunctioning parathyroid allows us to perform a faster surgery and ensure a better recovery. If we can’t locate it with those two studies, we have 4DCT and expert radiologists who are skilled at reading the results.”
Dr. Jain sees many patients following unsuccessful parathyroid surgery. “The patient goes under anesthesia expecting to have a successful operation, and then wakes up to discover that it’s unfinished,” he says. “Surgeons who do high volumes of parathyroid surgeries produce better outcomes. When we use technology to localize the parathyroid, the incision is smaller, time in the OR is shorter, and recovery is faster.”
Lee remembers her experience as one of the most pleasant she’s had in a hospital. “Everyone at the hospital treated me with the utmost respect and care,” she says. “I think very highly of Dr. Jain and am glad I went ahead and had the surgery done. Things are back to normal.”